By Debbie Bunch
May 19, 2025
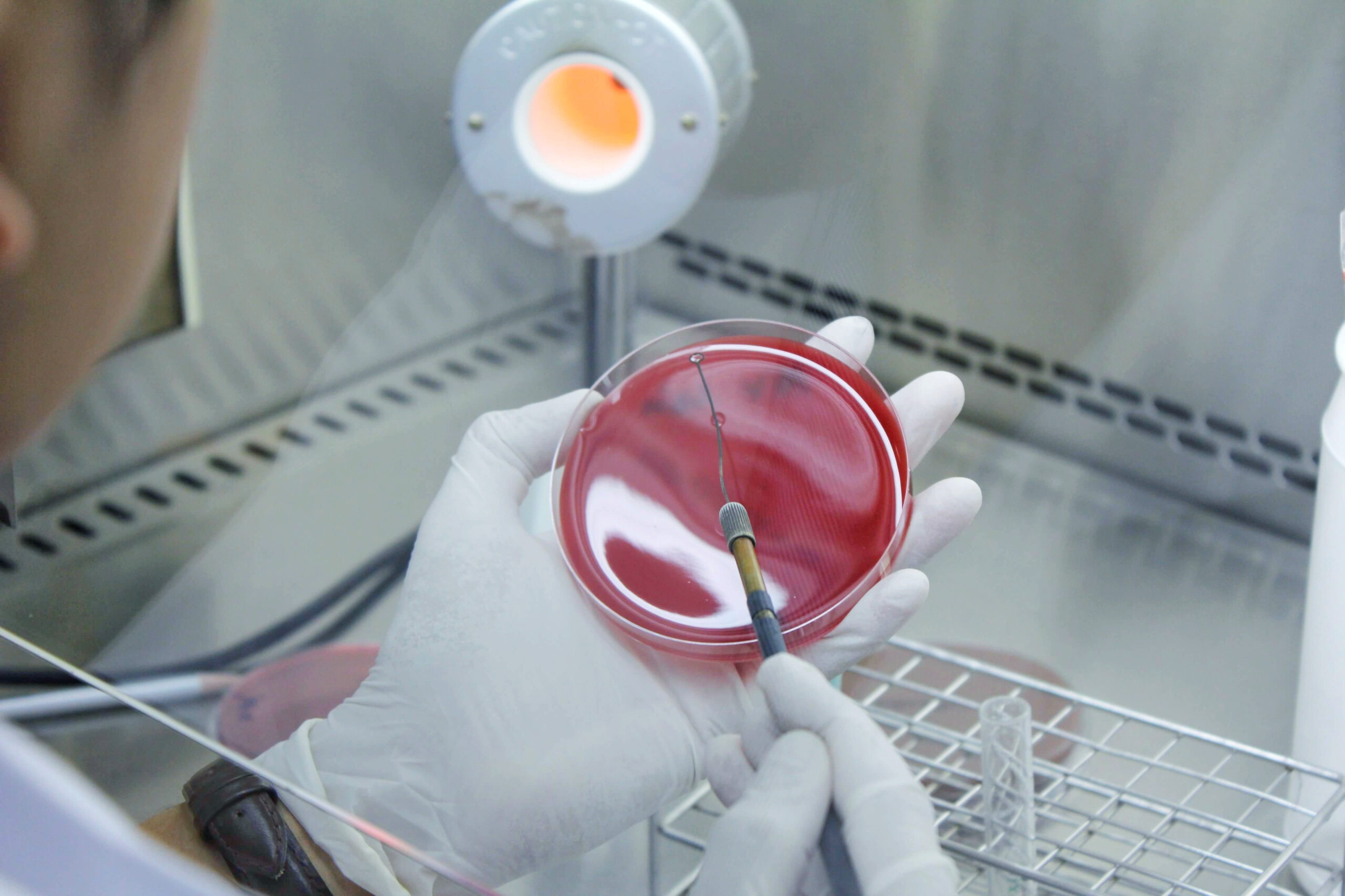
Phage Therapy Holds Promise for CF Patients
Antimicrobial resistance is considered a global health threat, especially for vulnerable populations like those with cystic fibrosis. Researchers from the Center for Phage Biology and Therapy at Yale University believe they may have found a way to overcome the problem.
The study employed phage therapy, which uses viruses (also known as phages) to target and kill bacteria, to treat nine adults with CF who were not responding to standard cystic fibrosis therapies. The therapy was personalized for their specific conditions and delivered via nebulization.
Results showed:
- Five to 18 days after phage therapy began, sputum Pseudomonas decreased by a median of 104 CFU ml−1, or a mean difference of 102 CFU ml−1, without altering the sputum microbiome.
- An analysis of sputum Pseudomonas showed evidence of trade-offs that decreased antibiotic resistance or bacterial virulence.
- An improvement of 6% (median) and 8% (mean) predicted FEV1 was observed 21-35 days after phage therapy, which the authors believe may reflect the combined effects of decreased bacterial sputum density and phage-driven trade-offs.
- No adverse events were noted from the therapy.
“We currently have a lack of effective antibiotics, and the World Health Organization predicts that by 2050, we’ll have more deaths from antimicrobial resistance than from chronic diseases like cancer and diabetes,” said study author Jon Koff, MD, who is medical director of the Yale Center. “This compassionate treatment is an opportunity for us to use phage therapy for patients with life-threatening infections and no other treatment options.”
The center’s director, Paul Turner, PhD, acknowledges that infecting bacteria may be capable of evolving resistance to administered phages but believes Dr. Koff has the understanding necessary to deal with that likelihood.
“He continues to advocate that personalized treatments and clinical trials in phage therapy must address this possible limitation, so that evolved phage resistance in bacteria is either minimized or steered down a path which coincides with reduced pathogenicity, thus improving patient outcomes,” said Dr. Turner.
The team is currently in discussions with the CDC and the Cystic Fibrosis Foundation to set up phage treatment centers for CF patients across the country and is also working with countries in Europe and South America to establish phage programs there.
“When we look at the trajectory of antimicrobial resistance, we see a pandemic that could happen in the next 30 years,” said Dr. Koff. “By using phage therapy to help patients with cystic fibrosis, we are also finding solutions to address a growing crisis.”
The study was published in Nature Medicine. Read Press Release Read Full Paper

Predicting Pneumonia Severity in Kids
A recent study conducted through the International Pediatric Emergency Research Network offers some insights into which children will require hospitalization for pneumonia and care in the ICU.
“While only a small percentage of children with pneumonia will have severe outcomes, it’s crucial to identify these patients early so clinicians can act swiftly and aggressively to prevent further deterioration in these children,” said lead author Todd Florin, MD, MSCE, from Ann and Robert H. Lurie Children’s Hospital of Chicago. ”It is also important to know if the illness will likely be mild, in order to avoid potentially unnecessary tests or treatments or unnecessary hospital stays.”
More than 2,200 kids, ranging in age from three months to 14 years, who sought care for community-acquired pneumonia in 73 emergency departments in 14 countries were included in the study. The researchers found that children with a runny nose and congestion were more likely to have a mild illness. Clinical features associated with moderate or severe pneumonia included:
- Abdominal pain
- Refusal to drink
- On antibiotics for the current illness before the ED visit
- Chest retractions
- Respiratory rate or heart rate above the 95th percentile for age
- Hypoxemia
The researchers also included models in their study aimed at predicting pneumonia severity in kids for whom pneumonia was present on chest radiographs. They found that, in addition to the clinical features linked to more severe disease noted above, the risk of more severe illness rose when multiple regions of the lung were affected.
The authors believe that since the clinical features outlined by their study are routinely assessed in children, the model should be both generalizable and easy to implement.
“Emergency departments around the world see thousands of children with pneumonia every day, but until now, we haven’t had a reliable way to predict who’s truly at risk of getting sicker,” said co-author Nathan Kuppermann, MD, MPH, from the Children’s National Research Institute in Washington, DC. “This model gives clinicians a practical tool, rooted in data, to guide that decision and ultimately improve care and outcomes.”
The study was published in Lancet Child and Adolescent Health. Read Press Release Read Abstract

BPD Linked to Ciliary Dysfunction
Researchers from UT Health Houston have found that infants with more severe bronchopulmonary dysplasia (BPD) are more likely than infants with less severe BPD to show signs of ciliary dysfunction.
The investigators believe this is the first study to find a link between the two conditions.
“Ciliary dynamics have never really been studied before in BPD, and we found they can have a significant impact on the pathophysiology,” said first author Daniel A. Yassa, MD, a pediatric pulmonologist at UT Health Houston.
Dr. Yassa and his colleagues found the association between BPD and ciliary dysfunction through a high-speed video microscopy study to observe nine infants’ nasal samples. All the infants had BPD, and four recordings were analyzed for each infant.
A distinct reduction in the angle and amplitude of cilia beats was seen in infants with severe BPD, compared to those with more moderate disease, pointing to a potential role for mucociliary clearances in developing BPD.
The study authors believe these findings will lead to a better understanding of BPD and help classify diagnoses. New therapeutic targets could also emerge from the results. To further define the influence of ciliary dynamics on BPD, follow-up studies involving larger cohorts and advanced imaging techniques are being conducted.
The study was presented at the recent American Thoracic Society meeting. Read Press Release Read Abstract








