
By Debbie Bunch
June 2, 2025
Thirdhand Smoke Puts Children with Asthma at Risk
Ensuring that kids — and especially kids with asthma — are not exposed to cigarette smoke is essential in keeping them healthy. But what if the kids live in a household where no one smokes? Can they still be exposed?
According to U.S. researchers, the answer is yes. When they surveyed the parents of 162 children living in federally subsidized public housing in New Orleans, Cincinnati, and Boston, 60% said their children had zero exposure to environmental tobacco smoke (ETS), commonly known as secondhand smoke.
When those children were tested for urinary cotinine (UC) levels, however, the researchers found that 100% tested positive, and more than 90% tested positive for intermediate levels. Little variation in ETS exposure was seen in the children over the three data point collections that took place during the one-year study.
What’s going on? The investigators believe the children were exposed to a less well-known type of ETS called thirdhand smoke. Thirdhand smoke is the smoke that remains embedded in carpets, walls, and furniture long after smoking is banned from a home. Studies suggest it becomes more toxic over time and resists conventional cleaning methods.
Given the levels of UC found in these children, whose parents said they did not allow smoking in their homes, the researchers also believe using surveys to assess ETS exposure in kids may not be the best practice. Assessing for biomarkers like cotinine may be more effective. In this study, for example, high levels of cotinine in kids with asthma were linked to the prevalence of asthma attacks, but no association was seen between caregivers who reported ETS exposure for their children and asthma attacks.
“These findings do not imply that the parents are lying but rather speak to the invasive nature of thirdhand smoke and how difficult it is to remove from buildings, cars, and furniture,” said study author Katherine McKeon, from Tulane University. “Thirdhand smoke is a newer concept, but ongoing research points to it posing a highly toxic silent threat to children, particularly to children with asthma.”
The study was published in the Journal of Clinical and Translational Science. Read Press Release Read Full Paper

New Diagnostic Schema for COPD Picks Up Missed Cases
Researchers from two major COPD research groups believe they have developed a more effective way to diagnose the disease.
Their new COPD diagnostic schema, which includes chest imaging, respiratory symptoms, and spirometry, was tested in 10,305 participants in the COPDGene study and 1,521 participants in the Canadian Cohort Obstructive Lung Disease (CanCOLD) study.
The multidimensional schema is based on a major diagnostic category, which includes the presence of the primary criterion (airflow obstruction based on postbronchodilator FEV1/FVC ratio <0.70 and at least one of five minor criteria (emphysema or bronchial wall thickening on computed tomography, dyspnea, poor respiratory quality of life, and chronic bronchitis); or a minor diagnostic category, which includes the presence of least three of five minor criteria (which must consist of emphysema and bronchial wall thickening for individuals with respiratory symptoms potentially due to other causes).
The primary outcomes and measures included all-cause mortality, respiratory cause-specific mortality, exacerbations, and annualized change in FEV1. The authors found:
- Reclassified individuals with a new COPD diagnosis had greater all-cause mortality and respiratory-specific mortality, more exacerbations, and more rapid FEV1 decline compared with individuals classified as not having COPD.
- Among individuals with airflow obstruction on spirometry, those no longer classified as having COPD had outcomes similar to those without airflow obstruction.
- Among 1,341 adults in CanCOLD, individuals newly classified as having COPD experienced more exacerbations.
“Using two large multicenter longitudinal cohorts of adults with varying risk of COPD, this study demonstrated that, compared with use of the GOLD diagnostic criteria for COPD, application of a new multidimensional COPD diagnostic schema resulted in inclusion of additional individuals with high mortality and respiratory morbidity and exclusion of individuals with airflow obstruction on spirometry without symptoms or evidence of structural lung disease,” wrote the authors. “This new schema anchors the diagnosis of COPD to spirometry, if available, and includes additional elements (dyspnea, respiratory quality of life, and CT findings) to meet criteria for a COPD diagnosis.”
JAMA published the study. Read Full Paper
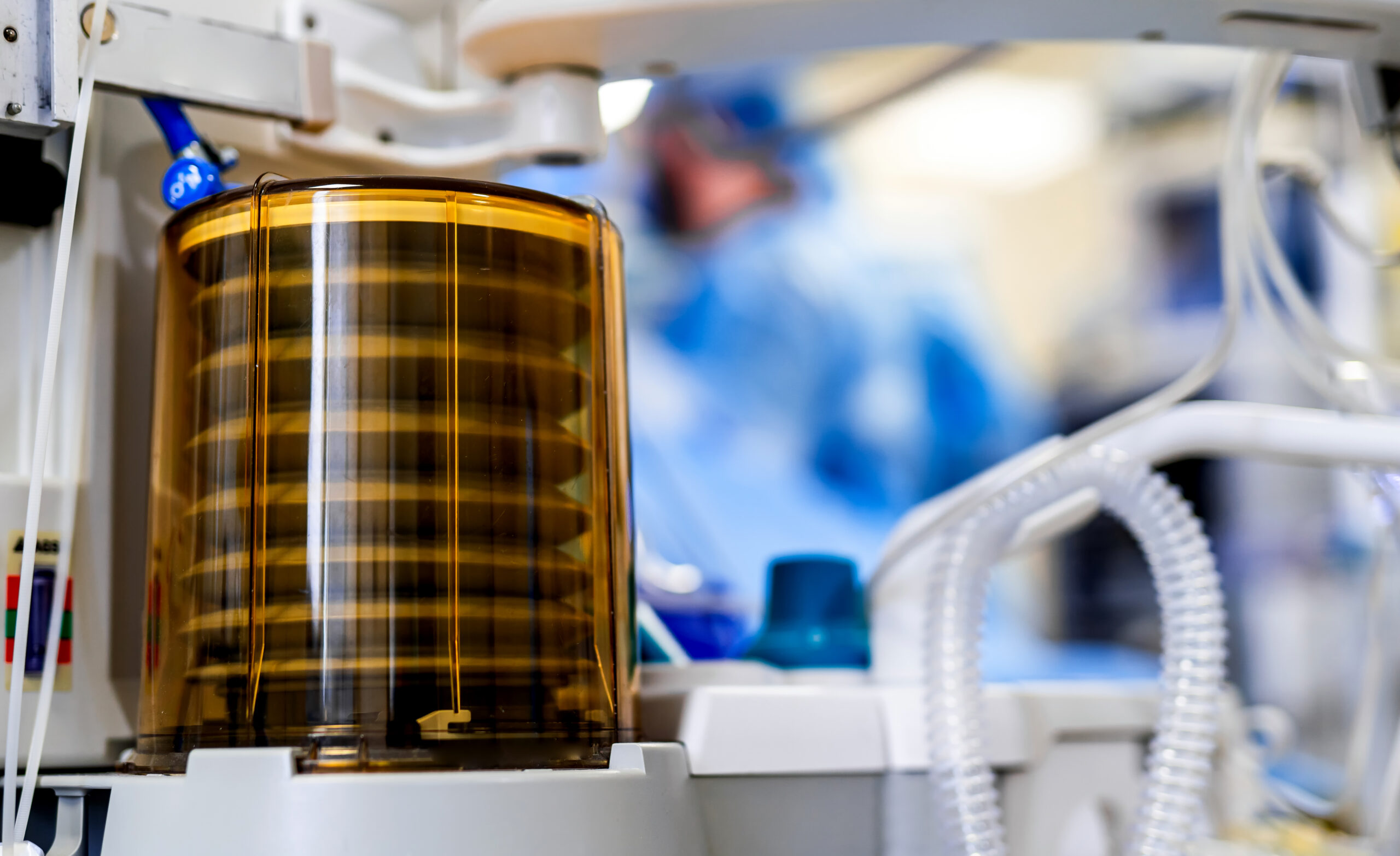
CDS Tool Improves Ventilator Outcomes for Kids
Can a computerized decision support (CDS) tool improve outcomes for children who require mechanical ventilation? Researchers from Children’s Hospital Los Angeles asked that question in a study that compared outcomes for 248 children with lung failure who were on mechanical ventilation at some point in their hospitalization.
According to the authors, the CDS recommends frequent adjustments to ventilator settings according to shifting patterns in patients’ breathing to stay within recommended ranges. In the study, patients were randomized to receive mechanical ventilation delivered by a lung- and diaphragm-protective CDS tool or to the usual standard of care, defined as ventilator management directed by their physicians without the aid of a CDS tool.
The seven-year study showed:
- The intervention patients had shorter weaning from ventilation — a median of 0.09 days compared to 1.04 days for patients in the control group.
- The interventional group also appeared to retain more respiratory muscle strength at the first standardized spontaneous breathing trial. It seemed to have a better functional status at ICU discharge than the control group.
“This is the first trial in either adults or children to test a computerized ventilation strategy that we had theorized could help preserve lung function and respiratory strength in children,” said lead study author Robinder Khemani, MD, MSCI. “When these children left the intensive care unit, they seemed less debilitated than the children who received usual care. It may mean that they had fewer negative effects caused by the ventilator with this approach.”
The authors believe Phase III trials in mechanically ventilated patients are warranted to further study the use of CDS in this patient population. NEJM-Evidence published the study. Read Press Release Read Full Paper








